Sleep is the Key to Mental Wellness
When did we start regarding sleep deprivation as a superpower? Sleep has a massive impact on overall mental health, and if you are diagnosed or experiencing a mood disorder—including anxiety, depression, bipolar disorder, or others—too much or too little sleep may be a cause or symptom of an emotional disturbance.
Note: Depression and other mood disorders can have critical consequences. Always seek help if you find yourself experiencing intense or prolonged feelings of hopelessness, anxiety, or emptiness. If you or a loved one are experiencing suicidal thoughts or considering suicidal action due to lack of sleep or other factors, contact the National Suicide Prevention Lifeline at 1-800-273-8255 for immediate assistance.
How Sleep Affects Mental Health & Mood Disorders
Are sleep problems a cause or an effect of mood disturbances? Clearly both. Many patients report experiencing sleep disruptions preceding or during mood disturbances. Examples include, but certainly are not limited to:
- Anxiety: Anxiety disorders can cause racing thoughts, elevated heartbeat, and panic attacks when trying to sleep, resulting in insomnia. Lack of sleep will increase fatigue, exacerbate concentration difficulties, and make managing the nervousness and overwhelming fear associated with these disorders challenging.
- Bipolar Disorder: Bipolar disorder is characterized by intense highs and lows. When experiencing mania, you may be unwilling or unable to sleep. Depressions may result in extreme fatigue and too much sleep. These inconsistent sleep patterns lead to difficulty regulating emotions.
- Depression: Depending on your diagnosed depressive disorder, you may experience insomnia or too much sleep. Both lead to heightened fatigue, brain fog, difficulty focusing, headaches, trouble maintaining an exercise routine, and challenges regulating emotional responses to various factors.
In addition to these disorders, too much sleep or insufficient sleep can have a noticeable impact on symptoms of adult ADHD, OCD, and other disorders. If you are experiencing new or worsening symptoms, improper sleep may be the culprit. But understanding how sleep affects mental health is only the beginning—now it’s time to make a plan to improve your sleep and enhance your quality of life.
How to Improve Your Sleep for Better Mental Health
Practice Good Sleep Hygiene
Sleep hygiene refers to healthy habits built to support better sleep. In our modern world, sleep hygiene means applying self-discipline and dedication. Consider these behaviors as you work to improve your sleep and positively affect your mental health through new habits:
- Turn off and put away all screens and electronics at least thirty minutes before bed
- Set and maintain a consistent bedtime
- Use relaxation or grounding techniques before going to sleep
- Avoid alcohol, tobacco, caffeine, and similar substances in the late afternoons and evenings
- Get regular exercise and natural light exposure during the day
Monitor Your Sleep
Documenting the relationship between disrupted sleep and mood disturbances can be a way to determine if the two are linked. Current and easily accessible technology, such as smartwatches and other wearable devices, make it convenient to collect your heart rate variability (HRV) during sleep. You can use this data to find patterns and discover if a link exists between your sleep and oncoming mood disruptions, then examine your behaviors to create an actionable plan that minimizes pending psychiatric episodes.
Keep in mind that subjective self-reports of sleep may not always be a reliable tool for mental health monitoring. Many people get exasperated tracking their habits, and sleep physiologists have found that self-reporting often differs drastically from professionally conducted sleep studies. If you cannot address your sleep disturbances independently, seeking professional assistance is your best step.
Seek Professional Assistance & Follow a Personalized Medication Plan
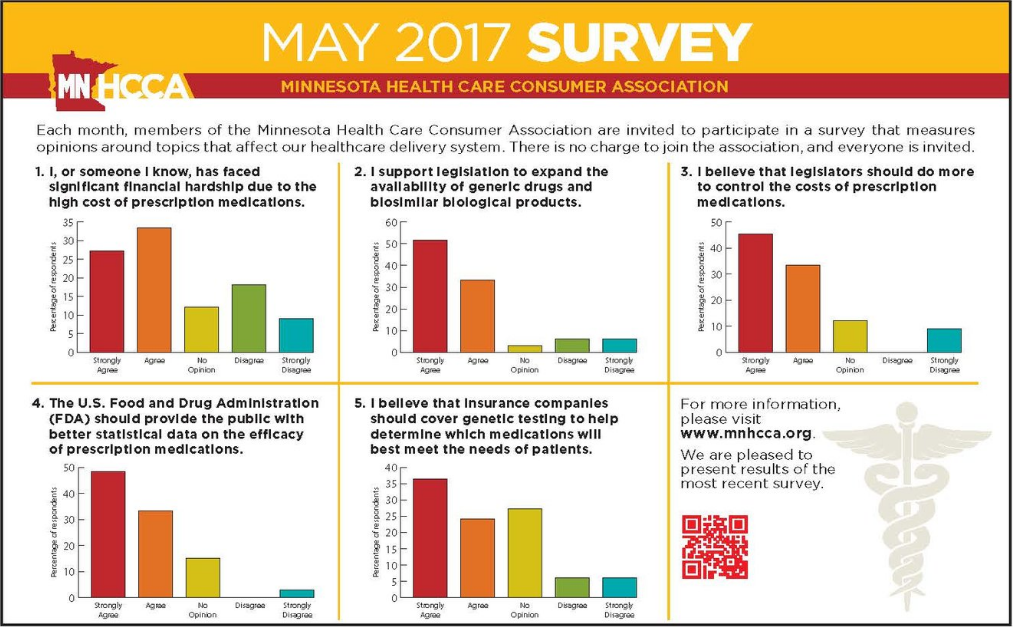
If you are unable to improve your sleep on your own, working with a professional is your best option. Psychiatric sleep specialists have the knowledge and capabilities to analyze your self-collected HRV rates, conduct in-office sleep studies, and create personalized treatment plans to improve your sleep and quality of life. One part of your plan may include new or adjusted medication. Medication management carried out by a qualified team can consist of:
- Lowering or raising does to ensure medication side effects are not causing too much or too little sleep
- Making changes proactively in response to early changes identified in observed HRV patterns
- Trying different medications to find the best solution for your unique symptoms
- Simplifying your medication regiment
- And more!
West End Consultation Group is Here to Help You Sleep Better & Improve Your Mental Health
West End Consultation Group is dedicated to creating individualized pathways to wellness through mental health treatment. If you or a loved one is experiencing disruptions in sleep or worsening mood disorders, our board-certified team is here to support you. We work with adult patients throughout the Twin Cities and are prepared to help you discover how sleep affects your mental health. Contact us today to learn more about our services and get started on the road to better mental health.
Medical Disclaimer:
Please remember that all medical information provided in this post must be considered educational only. This blog should not be relied upon as a medical judgement and does not replace a medical professional’s judgement about the appropriateness or risks of a procedure or condition for a given patient. We will do our best to provide you with information that may help you make your own healthcare decisions. Please do not follow any instructions or information without first consulting with your physician or mental health provider.