The Dangers of Online Prescribing
The number of online services offering subscription-based psychiatric medication prescriptions has increased substantially in recent years. These services often promise quick access to psychiatric prescriptions while marketing themselves as an affordable option. However, there are several reasons to be wary of online prescribing services for psychiatric medication.
Three Reasons to Be Cautious of Online Prescribing Services
1. The Lack of Face-to-Face Care
Online prescribing services are absent of the benefits that come with face-to-face care. With face-to-face care, a psychiatric professional can observe non-verbal signs and symptoms that provide a more complete understanding of the best solutions and medications. Fidgeting, shifting, nervousness, signs of anxiety, and other physical indicators can be identified through traditional in-person care. Prescribing services that are entirely virutal, on the other hand, fail to catch these qualitative and often non-verbal signs.
Online prescription services also miss the ongoing assessment and evaluation necessary for extended and personalized care. Instead, they rely on brief questionnaires and online check-ins for information about the patient. This approach simply does not provide enough information to paint a complete picture of a person’s individual and complex mental health needs. Without a full in-person assessment or ongoing support, there’s an increased risk of misdiagnosis or missing other underlying conditions that could affect treatment.
Additionally, some psychiatric medications require in-person evaluation in order to be prescribed. Due to these DEA restrictions, an entirely virtual prescriber is limited to the medications they can prescribe. When looking at many of the online prescribing platforms, they often have around five medications that they offer for each set of symptoms. Psychiatric care is not “one size fits all,” so limiting the medications and available resources can cause roadblocks in providing effective care.
Telehealth is a helpful tool that can increase accessibility to care and boost convenience. However, there must be a balance. Psychiatric care should allow for what is best for the patient and their treatment plan. Allowing for a mix of in-person and virtual face-to-face care works well for many patients. Some people benefit from entirely in-person appointments or require additional monitoring that must be done in-office.
2. A Higher Financial Cost
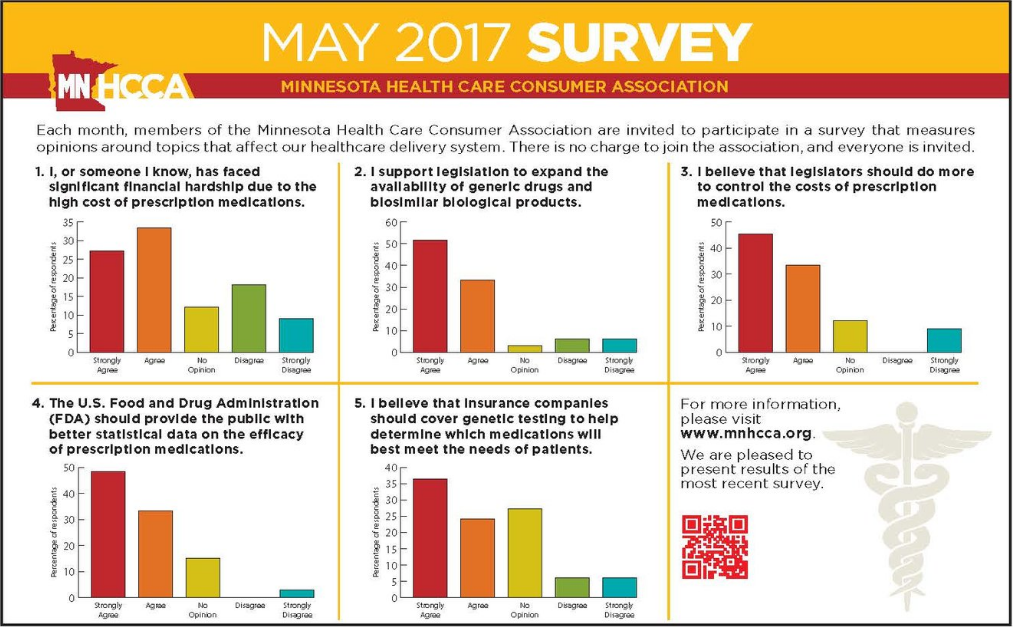
While many online subscription services portray themselves as a cost-effective solution for getting psychiatric medication, the reality is that over time, they typically end up costing far more than traditional pharmacies and psychiatric treatment services. These services generally do not accept insurance for the cost of the subscription. They also often include recurring fees, increased prices for medications, and additional charges for services not covered in the subscription. These costs all add up quickly.
For example, a typical appointment with a psychiatrist or psychologist might be covered by insurance, and medication costs can be minimized by using conventional options available at local pharmacies. In contrast, subscription-based prescription services often bypass insurance. Instead, people seeking psychiatric care end up paying out-of-pocket. These services also often push branded medications over generic medications, which can significantly increase the final price of care. All of this leads to higher overall costs.
3. Risk of Overprescribing or Prescribing the Wrong Medications
For many people seeking psychiatric treatment, there are often solutions other than medication that can produce positive results. Lifestyle changes, implementing healthy habits, and other solutions can often be part of a comprehensive psychiatric care plan. It is common for a comprehensive treatment plan to include both medication and lifestyle modifications, along with support in following the plan.
However, online prescription services might rush to simply prescribe medication without exploring additional treatment solutions. This one-size-fits-all method can contribute to overprescribing or the use of medications that might not be ideal for the individual. It also lacks the ongoing opportunity to assess the medication response or adjust the treatment plan based on the results over time. The result can be unnecessary side effects or dependency on medications that could have been avoidable with in-person care.
The Benefits of Personalized Psychiatric Care
In contrast to online subscription-based medication services, in-person psychiatric care offers numerous important advantages tailored to each person’s unique experience. Key benefits of in-person psychiatric care over online-prescribing services include:
- A personal connection with a psychiatric professional
- The opportunity for non-verbal interaction and observation
- Ongoing support and care built around your unique needs
- Increased likelihood that insurance will help cover medications and services
- Personalized medication management and treatment plans
- Mental health services tailored for adult ADHD, anxiety disorders, mood disorders, and more – not just a “one-size fits all” approach
Get In-Person Psychiatric Care that Meets Your Mental Health Needs
If you’re looking for psychiatric care and medication management services, West End Consultation Group can help. Our psychiatric professionals offer personalized care and mental health support designed to meet your unique needs. Contact our office in St. Louis Park, MN, today to learn more.